Contra Hoffman On Vitamin D Dosing
[epistemic status: pretty uncertain about each individual fact, moderate confidence in general overview]
I. Hoffman Contra Me
I’ve said many times that (to a first approximation) Vitamin D is a boring bone-related chemical. Most claims that it does exciting things outside of bones - cure COVID! prevent cancer! decrease cardiovascular risk! - are hype, and have failed to stand up to replication.
Ben Hoffman disagrees, and writes How To Interpret Vitamin D Dosage Using Numbers. I’m compressing his argument for space reasons; read the link to check if I’m still being fair:
I am sick of people rejecting good evidence about vitamin D because they are confused about the bad evidence and can’t be bothered to investigate, so I am going to explain it […]
Hunter-gatherers in the environment where most of our evolution happened might have been outside all day shirtless. On average the sun’s halfway from peak, so that might be equivalent to 8 hours of peak sunlight at the equator. [A study shows people in these conditions synthesize 400 IU of Vitamin D/5 minutes, which comes out to] 8000 IU per hour is 32,000 IU (800 micrograms) per day by this estimate.
When deciding how much is actually appropriate to supplement, we need to take into account diminishing returns; eventually the sunlight starts producing other secondary metabolites which are also good for us, so a 16,000 IU supplement is lower-quality than sunlight but similar in the effective dosage of the most important chemical our evolutionary ancestors’ bodies would have made from sunlight; in practice I wouldn’t take more than that.
Now let’s look at the object-level studies that Scott Alexander says show that vitamin D doesn’t work. I’m just going to look at the randomized controlled trials because observational studies for or against vitamin D are trash for anything except hypothesis generation unless they have a very carefully selected instrumental variable.
The colon cancer link is broken but the breast cancer study reports a dosage of 400 IU/day. On the exercise scale that’s FIVE MINUTES of brisk walking. FIVE MINUTES is not very long at all compared with FOUR HOURS. [An all-cause mortality study used a thrice-yearly dosing] that amounts to about 800 IU/day, or ten minutes of brisk walking on the exercise scale. [Other studies that found no effect of Vitamin D also used doses around this range].
[In the large Autier meta-analysis that found no effect overall, the highest dose studied was] 2000 IU (25 minutes), which is at least getting somewhere. Maybe that’s why “supplementation in elderly people (mainly women) with 20 μg vitamin D per day seemed to slightly reduce all-cause mortality.” […]
This is starting to get out of scope, and I’m not really interested in a conversation about whether Scott’s characterizations are honest, so I’m going to stop here. Let’s look for comparison at a study I liked.
The Spanish RCT studying vitamin D for COVID used a dosage regimen that - according to Chris Masterjohn’s summary - was “equivalent to 106,400 IU vitamin D on day one, 53,200 IU on days three and seven, and 53,200 IU weekly thereafter.” [Maybe the high doses explain why it found positive results unlike all the other studies].
In other words, a good day out in the sun produces 32,000 IU of Vitamin D, but studies mostly look at doses between 800 and 2000 IU daily. Maybe that’s why they find no effect.
I think this is probably not true, and that higher doses of Vitamin D would also be ineffective.
II. An Overview Of Vitamin D Dosing
Ben asks: if ancestral populations were getting tens of thousands of IUs of Vitamin D per day, why are we messing around with small doses like 400?
I think the answer is: ancestral populations aren’t actually getting that amount.
(before we go further, a technical point: some studies measure vitamin D supplement dose in ug, others in IU; one ug = 40 IU. Some studies measure serum concentrations in ng/ml, others in nmol/L; one ng/ml = 2.5 nmol/L. I will be using IU and ng/ml throughout for consistency’s sake, which means I may be “misquoting” some of the original papers (and there’s a risk I bungle the conversion). If you’re worried, double-check my work.)
Krzyscin 2016 tries to estimate how many IU the Hadza are getting from sunlight, and finds it’s 2,000, not 16,000. I can’t follow their reasoning fully, or figure out exactly where it diverges from Ben’s, but I think it involves them 1) avoiding the midday sun, and 2) being black.
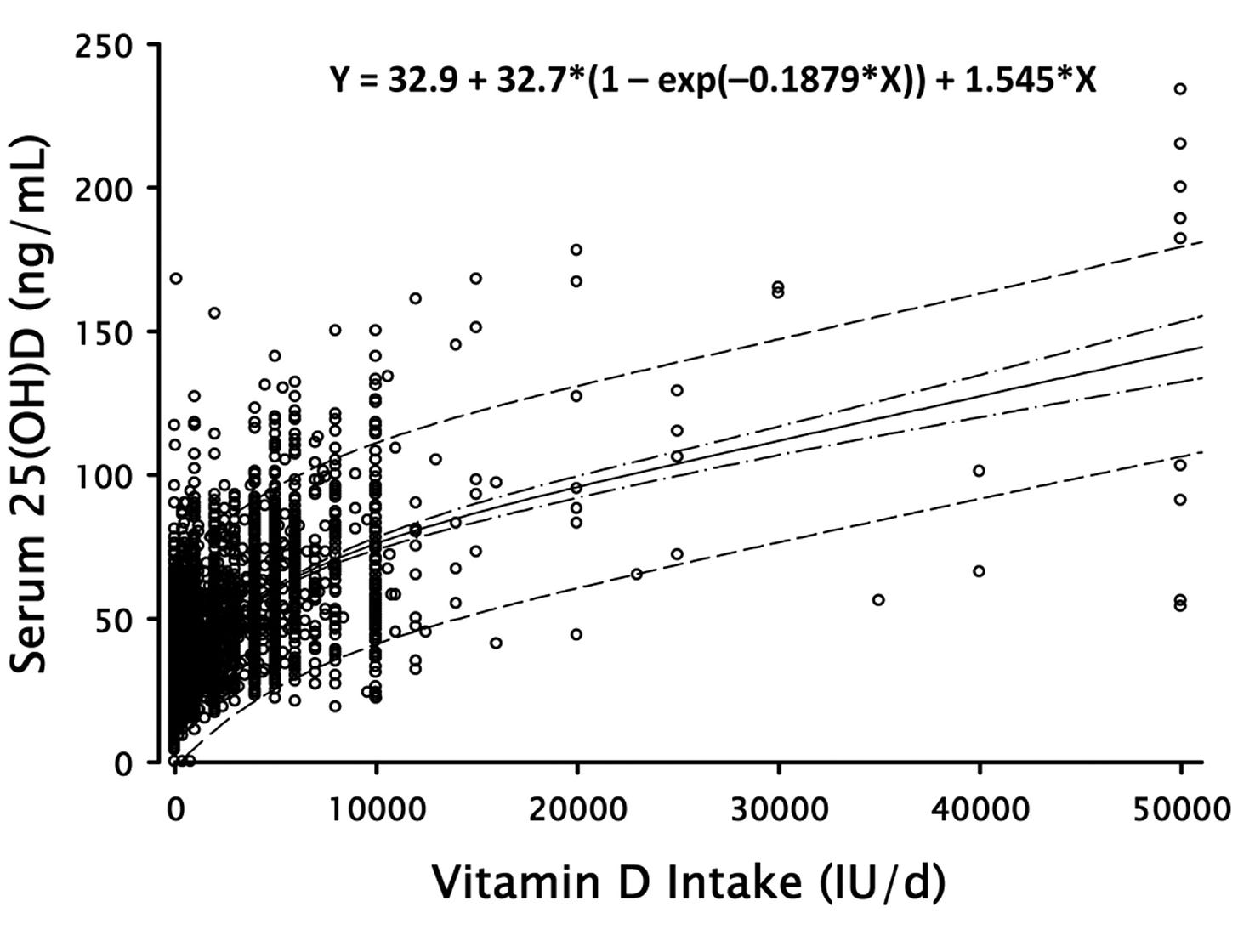
Luxwolda 2012 measured Vitamin D levels in the Hadza and found values from 28 to 68 ng/ml, averaging about 44. How many IU of Vitamin D supplementation would it take to get an average American to 44 ng/ml? Garland 2011 exists to answer this question for us:
It finds about 2000 IU, which makes no sense to me - Krzyscin said the Hadza were 2000 IU total , but Garland is saying that you need 2000 IU to get from current American levels (about 3/4 of the Hadza’s) up to the Hadza’s.
Dawson-Hughes 2005 says:
It is generally recognized that the increment in serum 25(OH)D in response to a given oral dose of vitamin D3 is inversely related to the starting level of 25(OH)D. The average increment in serum 25(OH)D has been estimated at 1.2 nmol/l for every mcg (40 IU) of vitamin D3 given as a daily oral dose at low starting serum 25(OH)D levels and only 0.7 or less nmol/l at the higher starting level of 70 nmol/l. Vitamin D2 gives a smaller increment of only 0.3 nmol/l for every mcg.
Suppose we’re starting from zero and want to get up to Hadza levels (44 ng/ml). 44 ng/ml = 110 nmol/L = ~110 ug Vitamin D = 4400 IU. This seems closer to Garland’s numbers than Krzyscin’s. I’m also more confident in these latter two estimates because Krzyscin’s seems really speculative and I’m not even sure I’m interpreting it right.
(Barger-Lux 2002 found that outdoor workers in Nebraska got 2800 IU from sun exposure, and yes, this is the second scientist in this essay studying sun exposure with “Lux” in their name)
In any case, probably hunter-gatherers like the Hadza are getting somewhere between 2000 and 4400 IU daily, not the 32000 that Ben attributes to them.
Bodekaer 2014 studies farmers in Denmark, who are usually outside most of the day, and find levels between 27 (in summer) and 18 (in winter). Acherjya 2020 finds that farmers in Bangladesh are around 30.
Surprisingly, average American levels seem about as high. The nationwide average is about 27 mg/nl, but black people (whose dark skin blocks sunlight) are almost all insufficient and bring down the average; for whites, it’s about 30 ng/ml. Why are these levels as high as some of the farmer-specific studies elsewhere? Maybe it’s Americans’ better nutrition - or maybe it’s that lots of Americans already take Vitamin D supplements. Canadians are close behind at 26 ng/ml; they fail to break this down by season but I’m guessing it was in the summer.
Various studies claim that 40% or 60% or 99% or 100% of Americans are “deficient in vitamin D”. These depend a lot on the exact standard you’re using, but a typical model of “deficiency” (technically insufficiency, you’re not supposed to use the word “deficient” unless there are observable health consequences) is an 18 ng/ml office worker.
Using the Garland model above, bringing that office worker up to the level of a Bangladeshi farmer would take 1200 IU. Bringing him up to the level of the Hadza would take 2600 IU. Bringing an average (not unusually deficient) American up to the level of the Hadza would take 1400 IU. All of these seem pretty close to the range of supplements used in studies (600 - 2000 IU).
III. Much More Nitpicky And Tedious Debates About Vitamin D Dosing
This isn’t especially related to Hoffman’s point, but I think the previous section would be incomplete without it.
The Institute of Medicine, the official US group that sets recommended daily allowances for vitamins, recommends that average adults get at least 600 IU of Vitamin D per day, corresponding to a blood level of 20 ng/ml. Most people get less than that from food, but that’s fine because they get the rest from sunlight; IOM says that only 5% of Americans are “at risk of deficiency” for Vitamin D as per their standard for blood levels (an additional 18% are “at risk of insufficiency”).
Veugelers 2015 claims to have found a statistical error in this calculation. Everybody needs different amounts of vitamins, so the IOM tries to set the recommended daily allowance at a level such that, if everyone ate that level, 97.5% of people would be getting enough. The IOM made a simple mistake and aggregated by studies rather than by individuals; under their proposed RDA, 97.5% of studies would have an average Vitamin D level that was enough. It’s much harder to get 97.5% of people to have enough, because some people - especially the obese - are much worse at processing Vitamin D than average. So what’s the right dose? Veugelers’ followup paper claims that there is no correct RDA: if you made everyone take enough Vitamin D that you were really sure 97.5% were getting enough, you could be equally sure that some people were getting too much and it was making them sick. He comes up with a method to balance out risks and benefits of more Vitamin D, and suggests “doses of 1885, 2802 and 6235 IU per day are required for normal weight, overweight and obese individuals respectively”.
(this isn’t ideal supplement dose: most people will get some Vitamin D through sunlight and food, so ideal supplement dose would be somewhat less than this)
As far as I know, nobody wants to argue that Veugelers is wrong, or defend the IOM recommendation. But even though it’s been almost ten years, the IOM hasn’t changed its recommendation yet. They cite Veugelers’ paper to support an unrelated point, so they’re clearly aware of it. As far as I can tell, they just seem to move very, very slowly.
(this correction doesn’t really affect my response to Ben above - the amount it takes to bring the average American to the average Hadza level is still whatever it is. This is just about what you do if you want to be sure of getting 97.5% of people the right amount.)
Meanwhile, Manson 2016 uses a similar argument to make the opposite point. They argue that all of these “40% of people are deficient in Vitamin D” studies are exaggerations. 40% of people don’t get the recommended daily allowance of Vitamin D. But the recommended daily allowance is what the 97.5th percentile of trouble-absorbing-Vitamin-D would need in order to not be deficient. The average person getting less than the RDA is just fine. This is a kind of nitpicky point, but if you were panicking about the Vitamin D deficiency crisis, it’s a good reason to panic much less.
Meanwhile , another medical organization only slightly less prestigious than the IOM, the Endocrine Society, has recommended a much higher Vitamin D level, for totally unrelated reasons. They recommend serum levels of at least 30 ng/ml compared to IOM’s 20 ng/ml, claiming that this was better at maximizing calcium absorption, lowering parathyroid hormone (an indicator of insufficient calcium absorption), and preventing falls in the elderly. You can read the IOM’s side of the argument here, and the Endocrine Society’s here. I haven’t looked into this in enough detail to determine who I agree with.
Some people recommend very very high levels of Vitamin D supplementation, for example this one arguing for a recommendation of 8000 IU. These numbers usually come from combining the Endocrine Society’s high target for Vitamin D with Veugelers’ point about wanting to catch 97.5% of people, minus his point about how you shouldn’t do that because it might cause toxicity. I have not looked into the (complicated, vehement) debate about whether medium-to-high doses (around 10,000 IU) of Vitamin D really do cause toxicity or not.
IV. Mortality Studies
Ben brings up the Autier meta-analysis:
“Autier looks at 172 randomized trials (!) and finds ‘Results from intervention studies did not show an effect of vitamin D supplementation on disease occurrence’”
The highest dosage mentioned in the abstract is 2000 IU (25 minutes [of sunlight]), which is at least getting somewhere. Maybe that’s why “supplementation in elderly people (mainly women) with 20 μg vitamin D per day seemed to slightly reduce all-cause mortality.” Also, a SIGNIFICANT REDUCTION IN ALL-CAUSE MORTALITY is a huge deal. That is the gold-standard outcome metric that everyone wishes their study was adequately powered to hit. Last time I checked statins don’t reach all-cause mortality significance and they’re widely prescribed.
Reducing all-cause mortality is great. But the specific cause of mortality that Vitamin D reduces is most likely bone issues, because Vitamin D is a boring bone-related chemical. The authors said:
The slight reduction in all-cause mortality in trials with moderate doses of vitamin D seems to be a robust finding. But gains in survival are mainly in elderly women living independently or in institutional care, who are likely to initially have a very low concentration of 25(OH)D with a substantial risk of falls and fractures.
Elderly women very often die by falling, breaking their bones, and being too weak and frail to recover. Stronger bones effectively prevent this. I agree with this, and so does the medical establishment, which already recommends that elderly people at risk of falls get checked for Vitamin D deficiency and supplement if they have it. This is not an argument that Vitamin D has profound extraskeletal effects, that the establishment is wrong about Vitamin D, or that you should take 16000 IU per day.
More relevant to Ben’s thesis (thanks to GJM for noticing this) the study finds that:
Vitamin D supplementation dose of less than [800 IU] per day had an effect on all-cause mortality that was equivalent to higher doses, which suggests that vitamin D dose is perhaps not very crucial to achieve a biological effect in patients likely to benefit from such supplementation.
Except elsewhere they say that:
Mortality reductions in trials that used doses of [400–800 IU] per day of vitamin D seemed greater than were reductions noted with higher doses.
I’m not sure why they flip-flop between “lower doses are better” and “lower doses are the same”, but either way, I don’t think this supports Ben’s claim that higher doses are better.
V. COVID Studies
Ben writes:
The Spanish RCT studying vitamin D for COVID used a dosage regimen that - according to Chris Masterjohn’s summary - was “equivalent to 106,400 IU vitamin D on day 1, 53,200 IU on days 3 and 7, and 53,200 IU weekly thereafter.” Some of these are heroic doses, and the dosage regimen hardly seems optimal, but this is for people who had already been hospitalized with COVID, a situation of acute illness where the body might be churning through a tremendous amount of vitamin D. (For similar reasons I’ve started taking vitamin C megadoses when I get sick, because several grams per day could easily make a big difference even though the much smaller doses in RCTs don’t.) On the exercise scale, this is equivalent to walking a double marathon on the first day, a single marathon on days 3 and 7, and weekly thereafter.
Intense, and not spaced out as much as I’d like, which is some evidence against the validity of the study - but neither obviously too small to make a difference nor spaced too far apart to be meaningful. I would expect better results from an equivalent daily dosage schedule. Masterjohn’s calculation: “If this were given as daily doses, it would be the equivalent of 30,400 per day for the first week, followed by a maintenance dose of 7,600 IU per day.”
I’ve already written a bit about why I don’t trust Vitamin D for COVID, including the Spanish study, here, and a new study seems to cast further doubt on it. Still, the studies that don’t work don’t have as high a dose as the ones that do (except for this one, which is small - h/t Ben for pointing it out). Even if the Vitamin D doses used in most studies are physiologically reasonable (which is what I’ve been trying to prove in this essay), isn’t it possible that unreasonably high doses of Vitamin D still treat COVID?
Yes, it’s possible. But we should start from a very low prior.
Suppose I threw a dart at the Giant Chart Of Metabolic Pathways and hit a random chemical. I don’t have a dart, but I do have a mouse cursor, and I tried this and got “hydroxymethylbilane”, which sure does sound like a chemical. What are the chances that hydroxymethylbilane supplementation would treat COVID, prevent cancer, prevent cardiovascular disease, and lower all-cause mortality. Pretty low, right? Our priors on a random chemical doing that have to be less than 1%, or we get caught in weird logical traps.
Some people originally thought Vitamin D did all those things. They mostly thought this on the basis of studies, done at low doses, which found that it did. Those studies mostly found that it did because they confused correlation and causation (sicker people have less vitamin D). Then we did better studies (still at low doses) which found that none of those things were true after all, at least at the low doses which the studies investigated.
If we then say “Yeah, but it could still be true at higher doses”, we’re missing the point. Now that our original reason for thinking it’s true is no longer valid, we should be back to our prior for any given random chemical, like hydroxymethylbilane.
I’m being a little unfair here. We have a few extra reasons to prefer hypotheses about Vitamin D to those about other random chemicals. There are Vitamin D receptors on immune cells, the body sure does seem to go to a lot of trouble to get Vitamin D, and we get less Vitamin D now than we did in the evolutionary environment so maybe we’d do “better” if we were closer to the design specs.
Still, none of those really seem that convincing to me - most of them are true of Vitamin E, Vitamin K, etc, and everyone just agrees those have their well-defined roles and probably don’t help COVID or cancer. Even among vitamins with widespread deficiencies, our prior should be pretty low.
I think the strongest reason people keep looking for this kind of thing is that scientists published studies showing a lot of effects, people got very excited, and then they forgot to keep track of where that excitement came from, and it stuck around even after the original reason disappeared.
VI. Summary
I think, to a first approximation, that Vitamin D is a boring bone chemical. I say “a first approximation” because I accept there are Vitamin D receptors on immune cells and a couple of other things, and it probably plays some role in modulating those. But it doesn’t seem to be a very big role, and I don’t think there’s much evidence for it having big effects on non-skeletal diseases within the normal or slightly-insufficient range.
Most Americans probably get a reasonable amount of Vitamin D that puts them in the healthy range. Some groups (elderly people, dark-skinned people, obese people, people who rarely go outside) are at higher risk than usual for insufficiency. People in this group might want to supplement. Reasonable levels of Vitamin D supplementation are probably somewhere between 500 and 5,000 IU, towards the higher end of this range for the obese. A bunch of very knowledgeable experts and doctors like having extremely protracted fights about where in that range is exactly optimal. If you want to go higher in that range, you can trade off a tiny mostly-theoretical risk of a very mild insufficiency for a tiny and mostly-theoretical risk of a very mild toxicity. I don’t know which of these is higher, and the 1 micromort or whatever that I could gain by getting this question exactly right doesn’t make it seem worth my time to investigate.
Although some small percent of the population needs very large Vitamin D doses, the doses used in studies are probably appropriate for most people, and the results of those studies are probably trustworthy (aside from all the usual reasons why study results might not be trustworthy, of course).