Oh, The Places You'll Go When Trying To Figure Out The Right Dose Of Escitalopram
I.
What is the right dose of Lexapro (escitalopram)?
The official FDA packet insert recommends a usual dose of 10 mg, and a maximum safe dose of 20 mg. It says studies fail to show 20 mg works any better than 10, but you can use 20 if you really want to.
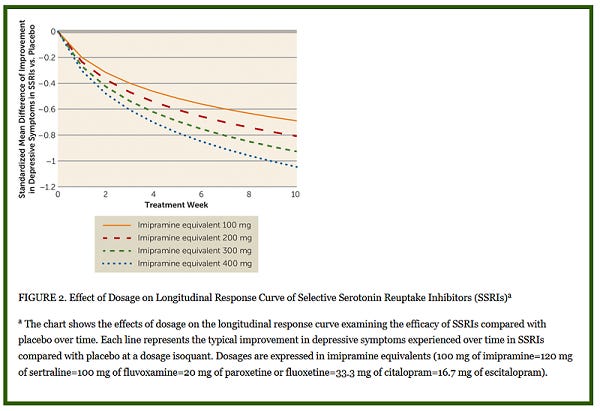
But Jakubovski et al’s Dose-Response Relationship Of Selective Serotonin Reuptake Inhibitors discusses which doses of which antidepressants are equivalent to each other, and comes up with the following suggestion (ignore the graph, read the caption):
[update: a commenter notes that Jakubovski’s equivalencies here are basically made up. I’m not completely tossing this out because I think they reflect a sort of consensus opinion, but that consensus might just be wrong].
16.7 mg Lexapro equals 20 mg of paroxetine (Paxil) or fluoxetine (Prozac). But the maximum approved doses of those medications are 60 mg and 80 mg, respectively. If we convert these to mg imipramine equivalents like the study above uses, Prozac maxes out at 400, Paxil at 300, and Lexapro at 120. So Lexapro has a very low maximum dose compared to other similar antidepressants. Why?
Because Lexapro (escitalopram) is a derivative of the older drug Celexa (citalopram). Sometime around 2011, the FDA freaked out that high doses of citalopram might cause a deadly heart condition called torsade de pointes , and lowered the maximum dose to prevent this. Since then it’s been pretty conclusively shown that the FDA was mostly wrong about this and kind of bungled the whole process. But they forgot to ever unbungle it, so citalopram still has a lower maximum dose than every other antidepressant. When escitalopram was invented, it inherited its parent chemical’s unusually-low maximum dose, and remains at that level today [edit: I got the timing messed up, see here]
Now that we know the heart risk was overblown, should we increase the maximum dose to something closer to other SSRIs? Maybe not. Right now, escitalopram keeps showing up in studies and head-to-head comparisons as the most effective SSRI.
But if we’re kind of under-dosing it, why should it work so well?
II.
The first reason Lexapro might work so well despite its low dose is that we’re prescribing too-high doses of every other SSRI for no reason.
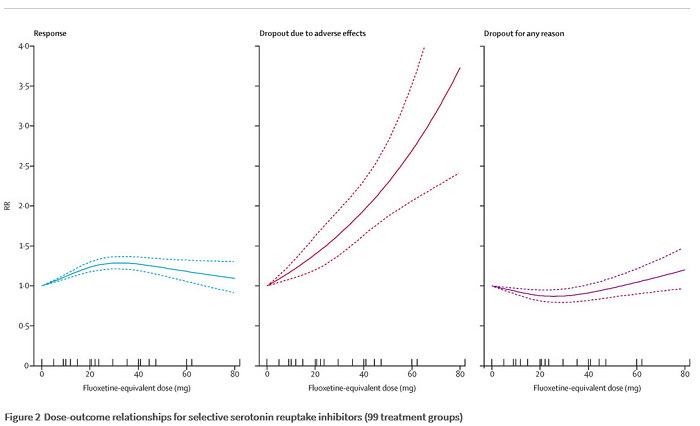
That’s the controversial conclusion of Furukawa et al. They use the giant database of antidepressant studies that Cipriani collected for his big meta-analysis, and examine all “fixed-dose studies” (we’ll return to this term later). Their key finding is this:
They find antidepressants are most effective (the first graph, marked “response”) at doses equivalent to 30 mg of fluoxetine (aka Prozac; 1 fluoxetine-equivalent = 5 of the imipramine-equivalents the other study uses). If that were true, the most effective dose of every SSRI would be:
Prozac: 30 mg
Paxil: 30 mg
Zoloft: 75 mg
Celexa: 30 mg
Lexapro: 15 mg
Other antidepressants are more complicated and you probably shouldn’t extrapolate to them. But this provides a simple explanation for why Lexapro does so well despite the low dose cap - we are overdosing everything. In this picture, there is no benefit to going above a low-to-medium dose of antidepressant. In fact, it looks like going above this dose makes things worse rather than better. Anyone who actually prescribes the FDA-approved maximum dose of Prozac 80 mg is making things worse for no reason.
Is this true?
In a polite but scathing editorial in the Lancet, Dr. Fredrik Hieronymus argues that it isn’t. He points out that Furukawa et al used “fixed-dose trials” - studies where researchers decide how much of a drug their subjects will take, then give it to them good and hard. Many of these studies don’t involve titration - the process of starting at a low dose, then working your way up gradually. Most real doctors do titrate, because starting someone on a high dose right out of the gate usually causes really bad side effects. So these studies make high doses look unnaturally bad.
But wouldn’t this show up as unexpectedly high side effect burden at high doses, and not as unexpectedly low efficacy? Dr. Hieronymus doesn’t mention this, but it might not. Most studies use “intention to treat”, meaning that if you hate the drug and stop it immediately, you still get counted in the study results. So suppose you’re depressed and sign up for an antidepressant trial. They start you immediately on a very high dose of an antidepressant, without easing you into it at all. You get every side effect in the book, you hate it, you stop taking the medication, and you presumably stay depressed. Then when they record the trial, they note that you were in the active drug group, and you’re still very depressed. It looks like a failure for the active drug!
Do studies back this concern up? Sort of. We have Frequency Of Positive Studies Among Fixed And Flexible Dose Antidepressant Clinical Trials, which shows that studies where you actually take some time to figure out what dose a patient needs show better results than studies where you hit them immediately with random doses. But the details here are really confusing and seem to mostly involve differences in the placebo group that don’t make sense. Overall I don’t have much confidence in it.
I think the conclusion I draw from all of this is that it’s possible that high dose antidepressants are no better than low-to-medium dose, but that this hasn’t been proven completely to my satisfaction.
III.
The second reason Lexapro might work so well despite its low dose is that it’s just better than other antidepressants. So good that even a little bit of Lexapro is as good as a lot of something else. This is the position suggested by Sanchez, Reines, and Montgomery (2014).
Obviously our first question should be whether Sanchez, Reines, and Montgomery all work for the company that manufactures Lexapro. The answer is: Sanchez and Reines definitely do. Montgomery says he doesn’t, but you can choose whether or not you want to believe him. On the other hand, by 2014 Lexapro was off-patent and the company could no longer make much money off of it, so I’m having trouble figuring out what their angle is here. Maybe just pride? I’m not sure. Still, let’s read the paper.
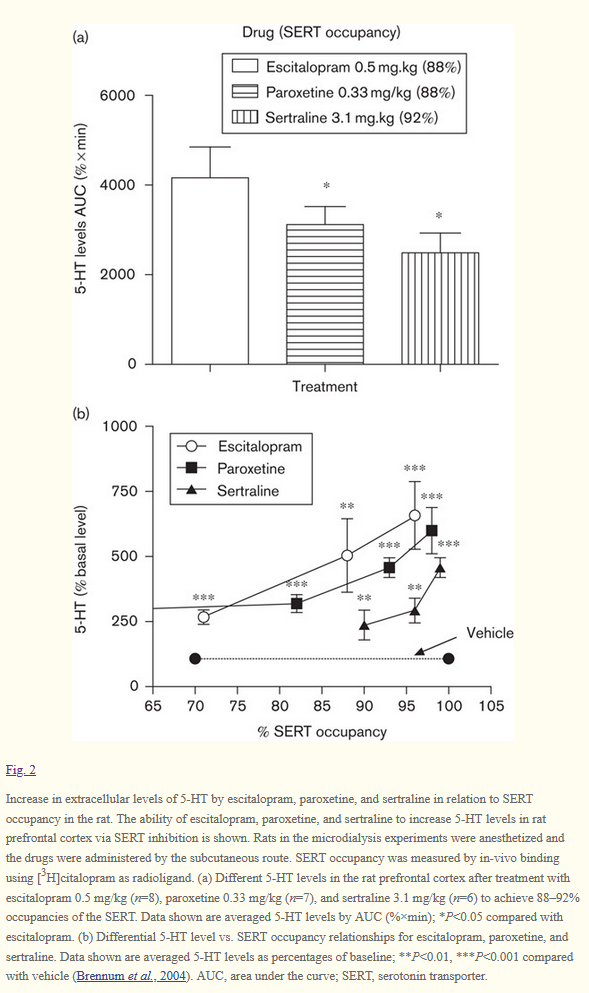
They note that other SSRIs only bind to the main site of the serotonin transporter and block it. Lexapro does this too, but it also binds to what’s called an allosteric site - a separate site which doesn’t block it, exactly, but changes its shape a bit. This means that although all SSRIs make the serotonin transporter work less well in one way, Lexapro makes it work less well in two ways. Because of this, Lexapro increases serotonin to a higher level than other antidepressants:
Sanchez, Reines, and Montgomery are so excited by this that they are willing to give Lexapro its own new class of medications, calling it not just an SSRI but additionally an ASRI (allosteric serotonin reuptake inhibitor). They claim they are taking this term from somewhere else but I cannot find it in any of their sources and I think Sanchez might have made it up in an earlier paper. There’s some interesting stereochemistry here where the s-enantiomer binds this site, the r-enantiomer prevents it from binding, and so the purely sinister escitalopram is more than twice as effective as the racemic mixture. For more on this, see Nutt and Feetam, What One Hand Giveth, The Other Taketh Away: Some Unpredicted Effects Of Enantiomers In Psychopharmacology. I hope the three of you who understand stereochemistry appreciate that title as much as it deserves.
This is pretty cool and could potentially explain why Lexapro seems to work a bit better than other antidepressants. But I don’t want to fall for it too quickly. Attempts to map the exact degree of serotonin increase to antidepressant effectiveness are fraught; vilazodone (“Viibryd”) seems to increase serotonin a lot more than any traditional SSRI, but doesn’t work any better. It’s all pretty mysterious. But maybe Viibryd increases serotonin in a mysteriously-bad way and Lexapro increases serotonin in a mysteriously-good way.
IV.
So that could explain why Lexapro works so well. If psychiatrists prescribed it at the same high doses as other antidepressants would it work even better?
I only know of three studies looking at this. The first is Wade, Crawford, and Yellowlees: Efficacy, Safety, and Tolerability Of Escitalopram In Doses Up To 50 mg In Major Depressive Disorder: An Open Label Pilot Study. Remember that the package insert says 10 mg is the recommended dose, Furukawa says 15 mg is the sweet spot, and the FDA says 20 mg is the maximum dose. So 50 mg is really high.
WC&Y got 60 depression patients and started them on Lexapro 10 mg. If they got better, great. If they didn’t get better, they kept increasing the dose to see what happened. They say that many patients who didn’t recover on normal doses of Lexapro did recover on high doses - their key finding was “38% of the 21 patients who achieved remission needed the 50 mg dose” - but this claim is totally unfair. They had no placebo group, and so can’t distinguish this from “38% of the patients who achieved remission needed a long time, and we kept raising their Lexapro dose while they waited”. The most that can be said about this study is that it’s consistent with high doses of Lexapro working well. In terms of safety, they found that Lexapro was well-tolerated with few side effects up to a dose of 35 mg, and kind of iffy after that.
The second study is Qi, Gevonden, and Shalev, Efficacy And Tolerability Of High-Dose Escitalopram In Posttraumatic Stress Disorder. They found basically the same thing - some of their patients who didn’t respond on low doses of Lexapro seemed to respond on high doses, but without a better study design we can’t tell if this is just because they waited longer. They found the medication was well-tolerated with few side effects up to 40 mg.
The third study is Rabinowitz, Baruch, and Barak, High Dose Escitalopram For The Treatment Of Obsessive Compulsive Disorder. Basically the same story, and possibly not relevant given that OCD may need higher doses than depression. But it’s useful as a sanity check, and it confirms that high-dose Lexapro was pretty well-tolerated. It also says one patient got manic on 45 mg Lexapro, which is too bad for the patient but otherwise a good sign - accidentally making bipolar people manic is sometimes considered a sign that an antidepressant is working. The mania stopped after bringing the Lexapro down to 30 mg, which suggests the 45 mg dose really was doing something the 30 mg dose wasn’t.
I will add my own anecdotal evidence here, which is that I had a patient who spent a year pretty depressed, got very modestly better on Lexapro 20 mg, and agreed to let me experiment with higher doses of Lexapro on him. He got better still at 30 mg, and even better when we increased to 40 mg. I am relatively confident these were real effects.
Overall, I think there we’re on shaky ground saying that any antidepressant works better at high doses than low-to-medium ones of about 30 mg fluoxetine equivalent. But despite what the FDA says, prescribing high doses of Lexapro probably isn’t any worse than prescribing high doses of any other antidepressant, and it might even be better. In the rare cases where I think it might help, I plan to continue prescribing doses of up to 30 mg without worrying at all, and up to 40 mg while worrying only slightly.
Please consult with your doctor before changing your dose of Lexapro or any other medication based on something you read on the Internet.