Peer Review Request: Ketamine
I’m trying to build up a database of mental health resources on my other website, Lorien Psychiatry. Whenever I post something here, people have had good comments, so I want to try using you all as peer review.
This is a rough draft of my page on depression. I’m interested in any feedback you can give, including:
1. Typos
2. Places where you disagree with my recommendations / assessment of the evidence
3. Extra things you think I should add
4. Your personal stories about what things have or haven’t helped, or any extra insight that your experience with depression has given you
5. Comments on the organization of the piece. I don’t know how to balance wanting this to be accessible and easy-to-read with having it be thorough and convincing. Right now I’ve gone for a kind of FAQ format where you can only read the parts you want, but I’m doubtful about this choice.
6. Comments on the level of scientific formality. I tried to get somewhere in between “so evidence-based that I won’t admit parachutes prevent injury without an RCT” and “here’s some random stuff that came to me in a dream”, and signal which part was which, but tell me if I fell too far to one side or the other.
Ignore the minor formatting issues inevitable in trying to copy-paste things into Substack, including the headings being too small and the spacing between words and before paragraphs being weird. In the real page, the table of contents will link to the subsections; I don’t know how to do that here so it might be harder to read.
Here’s the page:
Ketamine
The short version: Ketamine is a new and exciting depression treatment, which probably works by activating AMPA receptors and strengthening synaptic connections. It takes effect within hours and works about 2-3x as well as traditional antidepressants. Most people get it through heavily-regulated and expensive esketamine prescriptions, or through even-more-expensive IV ketamine clinics, but evidence suggests that getting it prescribed cheaply and conveniently from a compounding pharmacy is equally effective. A single dose of ketamine lasts between a few days and a few weeks, after which some people will find their depression comes back; long-term repeated dosing with ketamine anecdotally seems to work great, but hasn’t been formally tested for safety. Some people also use ketamine-assisted psychotherapy, which is a very different form of treatment and can have impressive long-term results, but which is less explored and more idiosyncratic for each person.
The long version:
1. How can I get ketamine therapy?
2. How can I find a doctor willing to prescribe me ketamine?
3. How can my doctor prescribe me ketamine?
4. How safe is ketamine?
4.1: How concerned should I be about cognitive side effects of ketamine?
4.2: How concerned should I be about urinary side effects of ketamine?
4.3: How concerned should I be about hepatotoxicity from ketamine?
4.4: How concerned should I be about getting addicted to ketamine?
4.5: How concerned should I be about hypertension from ketamine?
5: How effective is ketamine?
6: Do I have to take ketamine IV? What about nasal and oral ketamine?
6.1. Do I have to take esketamine? What about regular ketamine?
7: What’s the right dose of ketamine?
7.1: What are the exact instructions for dosing ketamine correctly?
8: How long does ketamine work for? Do I have to keep taking it forever?
9: What is ketamine-assisted psychotherapy?
9.1: Where can I get ketamine-assisted psychotherapy?
9.2: Can I do informal ketamine-assisted psychotherapy on my own?
10. How does ketamine work?
11. Will you prescribe me ketamine?
1. How can I get ketamine therapy?
Getting access to ketamine is currently confusing, difficult, and expensive. There are three main routes you can use:
First, you can go to a ketamine clinic where an anaesthesiologist will inject you with IV ketamine. This has some real advantages: most of the studies have used IV ketamine, IV forms of any drug are usually the fastest-acting and most powerful, and this is the standard of care. It’s also expensive and annoying. A typical course would be six treatments over three weeks at $800 per treatment, for a total cost of $4800. Each session would take an hour or two, and require someone available to drive you back from the clinic afterwards. Insurance almost never covers this, and even if it works you may relapse after the three weeks and have to pay $4800 again. I appreciate the existence of these clinics but they’re not a realistic option for most patients.
Second, you can use Spravato. Spravato is an FDA-approved official ketamine spray. You won’t have get anything injected into your veins, and it’s a less “medical”-feeling experience than a clinic. But this has its own problems. Spravato isn’t exactly ketamine – it’s esketamine, a ketamine component, which might or might not work as well as regular ketamine. It’s only allowed in doses of 56 to 84 mg, which will be too low for many people. And it also costs about $6400/month and has to be administered in special clinics. The only saving grace is that some people’s insurances will cover this one after a lot of begging. I still don’t think it’s the best option for most people.
Third, you can just pick up pills of regular ketamine at a pharmacy for ~$10/dose, at whatever strength and schedule your doctor recommends, and take it at home, just like you do with any other medication. Why isn’t this method used more often? Because the ketamine they sell in pharmacies is officially approved for chronic pain. It’s totally 100% legal to use it for depression instead (this is called off-label prescribing), but because it doesn’t say “OFFICIALLY FOR DEPRESSION” on the label, a lot of doctors get confused and don’t want to prescribe it. Please consider using this method instead of spending your life savings on one of the others, then having no idea what to do when you need continued treatment.
2. How can I find a doctor willing to prescribe me ketamine?
There is no good answer to this question. Most doctors won’t do this, and the few who do usually charge a lot of money. If you’re willing to spend a lot of money, you can Google “ketamine clinic [your area]” or “psychiatrist who prescribes ketamine [your area]” and probably find someone.
If you already have a psychiatrist, consider asking them if they’re willing to prescribe ketamine. If they express interest but say they don’t know how to do it safely and effectively, consider referring them to this document.
If you’re a psychiatrist or other MD, please consider prescribing ketamine to appropriate patients without charging them a lot of money! This document will tell you how!
3. How can my doctor prescribe me ketamine?
They should look for a local compounding pharmacy that has ketamine available. Usually these places are easy to Google. Also, if they call up any compounding pharmacy in your area, that pharmacy should be able to say whether they dispense ketamine, and if not, refer them to one who does.
Ketamine may come in the form of a nasal spray or a troche (tablet you place under your tongue and let dissolve). I’ve listed some sample prescription regimens below in section 7 – your doctor can just write those on a prescription pad or send them through any e-prescription program.
4. How safe is ketamine?
I think pretty safe, when used responsibly. All drugs potentially have side effects, but at effective doses, ketamine’s are no worse than anything else’s.
People definitely feel unusual (sometimes bad) while experiencing the acute effects of ketamine. In Acevedo-Diaz et al’s study of ketamine infusions, over 80% of participants felt “strange, weird, or bizarre”; other popular adjectives included “spacey”, “woozy”, “loopy”, “floating”, and “numb”. I don’t consider any of these to be unexpected side effects; this is just what happens when you take a dissociative drug. That having been said, some people who take very low doses of oral or intranasal ketamine will avoid all of this. Also, some studies find rates of these feelings are no different on ketamine compared to placebo, maybe because people are pretty suggestible if you tell them they’re taking a drug that might make them feel weird.
There are common reports of severe side effects from recreational ketamine users, of which the best known are urinary (eg cystitis) and hepatic. It would be concerning if clinical use caused these at anywhere near the same rate. But we should remember that eg recreational amphetamine abuse produces all sorts of terrible side effects, but essentially none of them carry over to clinical amphetamine use (eg Adderall for ADHD). This is mostly because recreational users take doses orders of magnitude higher; “the dose makes the poison”.
For example, in one Chinese study of ketamine side effects, the recreational abusers had been using for an average of six years, 6.5 days a week, 3.5g / dose. That suggests a total lifetime burden of about 7000g of ketamine. For comparison, an average person who undergoes a course of ketamine infusion for depression receives about 8 doses of 35 mg each, for a total of about 3g of ketamine. It’s completely possible for 7000g of a substance to produce effects that 3g of the same substance doesn’t!
The four most concerning potential side effects of ketamine are cognitive effects, urotoxicity, hepatotoxicity, and hypertension. None of these concern me enough to stop prescribing normal doses of ketamine to appropriate patients. The rest of Part 4 is an explanation of why. Unless you’re really concerned about these side effects, feel free to skip it.
–4.1: How concerned should I be about cognitive side effects of ketamine?
Ketamine use causes acute distorted cognition for the next few hours. But there’s good evidence that this doesn’t lead to permanent damage at clinical doses.
From Side effects associated with ketamine use in depression: a systematic review:
In a study by Koffler and colleagues, 109 cognitive effects of ketamine in patients treated for chronic pain were extensively assessed with several neuropsychological tests before infusion and at 6 weeks post-infusion; they concluded that ketamine had no residual cognitive effects at 6 weeks. Murrough and colleagues reported that lowdose ketamine was associated with minimal acute neurocognitive effects in patients with treatmentresistant depression 40 min after ketamine infusion. They also reported that any changes in cognition appeared to be transient in nature, with no adverse neurocognitive effects 7 days after treatment. In both Koffler’s and Murrough’s studies, however, the followup periods were short, making it difficult to comment on longterm risks associated with repeated use.
A UK study compared frequent ketamine abusers to infrequent ones. The frequent group used an average of ~3 grams/day, at least four days a week, over several years. The infrequent abusers used about 1 gram/day, a few times a month, over several years. Although the frequent abusers had impaired cognition, the infrequent group didn’t. Both groups used much much much more ketamine than any clinical user would. This suggests that the threshold dose for long0term cognitive impairment is much higher than would be encountered in clinical use. Also, ex-ketamine users did as well as never-users, suggesting that even the impairments of high-dose ketamine use are not necessarily permanent.
–4.2: How concerned should I be about urinary side effects of ketamine?
This UK survey finds about 25% of recreational users experience some kind of urinary problem, and 3% had gone to their doctor about it (but there was no control group, so there’s no way of knowing how much of this was caused by ketamine vs. incidental).
In rats, 100 mg/kg of IV ketamine did not cause bladder inflammation, but 300 mg/kg does. Both of these are much higher than standard clinical doses, which usually range from about 0.5 – 3 mg/kg. This study did find that the lower dose caused interstitial nephritis, which as far as I know is not commonly a problem for humans.
Are there any reports of clinical users having urinary problems? Consensus Guidelines On The Use Of Intravenous Ketamine Infusions For Chronic Pain say they only know of a single case, the one reported in this Journal of Urology article. A 16 year old girl receiving 8 mg/kg oral ketamine for chronic pain developed various urinary symptoms; the ketamine dose was decreased to 2 mg/kg and they went away. However, the authors say they have seen three other such cases “briefly described on a palliative care drugs mailing list” (which I can’t access).
As far as I know, these four cases are the only known cases of cystitis from clinical ketamine use – out of all the thousands of patients over decades who must have received the drug. The 16-year-old – the only case where I have access to the details – was on a higher dose than ever gets used in psychiatry, and had brief, mild symptoms which went away immediately after going down to a lower dose. Based on these findings, I’m not especially concerned about urinary risk from ketamine with normal psychiatric use.
–4.3: How concerned should I be about hepatotoxicity from ketamine?
This is also common in recreational users. Does it happen at clinical doses?
Most of the work on clinical hepatoxicity has been done on chronic pain patients, who take very long ketamine infusions for complex regional pain syndrome. In the two cases reported by Zhu et al, liver injury began after 40-50 hours of continuous ketamine infusion, by which point patients had received 1000+ mg of ketamine. In the three cases reported by Noppers et al, liver enzymes were measured and found to be elevated after fifty hours, again after having received doses of ketamine in the 1000 mg + range.
Psychiatric ketamine infusions usually last one hour or less, and involve doses of 25 – 75 mg. As far as I know, there are no reports of liver injuries at these doses. LiverTox says:
In patients on oral antidepressants, liver test abnormalities were no more frequent with the addition of nasal spray esketamine than with placebo. In the pivotal trials of esketamine as therapy of treatment- resistant depression, mean serum ALT, AST and alkaline phosphatase levels decreased during active therapy and there were no reports of serum enzyme elevations, jaundice, hepatitis, discontinuations for serum enzyme elevations or serious hepatic adverse events. Although long term ketamine use is known to be associated with bile duct injury and episodes of cholestatic jaundice, esketamine has not been linked to a similar pattern of biliary injury or cholestatic hepatitis when used under medical supervision to treat depression. There has been little clinical experience with long term use of esketamine, but no instances of clinically apparent liver injury have as yet been reported with its use.
–4.4: How concerned should I be about getting addicted to ketamine?
There is no high-quality formal evidence about this topic. There are two case reports of patients getting addicted to normal doses of ketamine for depression (1, 2), though both are a bit unusual – one was a man who had been addicted to other prescription drugs before, another was an anaesthetist who self-administered. Remember that case reports often describe rare situations.
In general, I’m not very concerned about this with most patients, for a few reasons. First are the reports from expert prescribers, who say basically none of their patients ever get addicted. Second is the general experience of using addictive drugs in psychiatry – for example, amphetamine (Adderall), which despite its fearsome reputation as a street drug is rarely abused by patients who get it by prescription. Addiction is a biopsychosocial process and people without genetic and psychological predispositions to addiction are usually able to use these chemicals safely.
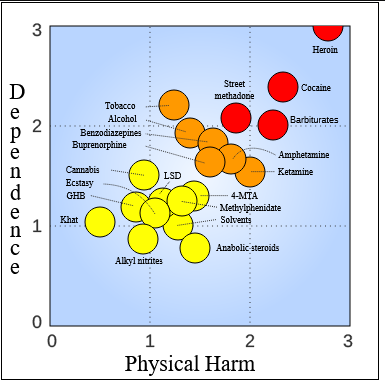
In a survey of drug experts, ketamine was ranked as less addictive than tobacco, alcohol, or Adderall, and around the same level as marijuana. If you would feel comfortable going out to a bar a few times without worrying about addiction, or smoking pot a few times without worrying about addiction, probably you also shouldn’t worry about getting a few ketamine infusions.
Long-term maintenance ketamine therapy has higher addiction risk, although still probably no higher than eg smoking marijuana regularly. One piece of good news is that there is no chemical dependence / withdrawal after coming off ketamine; any addiction is entirely psychological.
If you’ve gotten addicted to things before, or have a strong family history of drug addiction, or know that you have an addictive personality, you may want to avoid ketamine unless there are no other options. If you do get it, you might want to get it at a hospital or somewhere else where nobody is trusting you with your own supply of ketamine that you have to use responsibly.
–4.5: How concerned should I be about hypertension from ketamine?
Psychiatric doses of ketamine do cause transient hypertension, pretty often. UpToDate says that:
In four randomized trials, mean increases in systolic blood pressure ranged from 8 to 19 mmHg within 40 minutes of infusion, which normalized in four hours or less. In a pooled analysis of three randomized trials that included 97 patients who received a total of 205 infusions, the transient average peak increase was 20 mmHg.
How dangerous are these increases? They’re lower than the natural increase in blood pressure during heavy exercise (about 60 mmHg) or intense panic (30 mmHg).
A team from Emory University monitored blood pressure during ketamine infusions, with plans to stop if systolic blood pressure increased by 45 mmHg, or diastolic by 30, or if patients reported symptoms of severe hypertension (headache, chest pain, dyspnea, blurry vision). They did not have to stop any of 684 infusions.
If blood pressure increases too high, there is a small risk of a stroke, burst aneurysm, or other severe consequence. I would be wary about giving ketamine to patients who are already hypertensive, or at elevated risk for any of those conditions. For everyone else, transient minor hypertension probably isn’t such a big deal.
5: How effective is ketamine?
Pretty effective.
Studies find the effect of ketamine peaks about 24 hours after use. A meta-analysis finds that by that time around 50% of patients are feeling better (defined as 50% symptom reduction) compared to less than 10% of patients who got placebo. A more recent Taiwanese study finds roughly similar numbers.
Another way to measure effectiveness is through effect size statistics. The effect size of normal antidepressants like SSRIs is around 0.3. The effect size of ketamine is between 0.6 and 1.0, so about two to three times larger.
6: Do I have to take ketamine IV? What about nasal and oral ketamine?
As far as I can tell, there’s no clear advantage of IV ketamine compared to intranasal and oral.
Here I’m working off of The Effect Of Intravenous, Intranasal, And Oral Ketamine In Mood Disorders: A Meta-Analysis. Their data are hard to interpret, because different studies look at different time periods, and depending on what time period you choose, you can get different results. But in general, it shows about approximately equivalent efficacy for IV, IN, and PO ketamine (though they were hesitant to draw a firm conclusion about PO because of the small studies).
This tends to be the opinion of practitioners in the field too. I’m not sure why everyone insists on giving expensive, complicated, and potentially dangerous IV ketamine treatments when IN is right there.
–6.1. Do I have to take esketamine? What about regular ketamine?
No, take whichever.
What happened was: people did lots of studies showing that ketamine treated depression. But ketamine didn’t have an “OFFICIALLY FOR DEPRESSION” stamp on it, and couldn’t get it without pharmaceutical companies spending millions of dollars to clear bureaucratic hurdles. And no pharmaceutical company wanted to do that, because ketamine is cheap, common, public-domain, and impossible to make money off of. So instead a pharmaceutical company took a ketamine component called esketamine and spent millions of dollars to clear the bureaucratic hurdles for that one. Esketamine is patented, expensive, and only the specific pharmaceutical company involved is allowed to make it. But because it’s OFFICIALLY APPROVED FOR DEPRESSION, lots of official people, including the FDA and insurance companies, will prefer you use it.
There is no reason to think that esketamine is any better than regular ketamine. Some sources note that it has stronger NMDA antagonism, but NMDA antagonism is probably not ketamine’s main mechanism of action anyway (see section 10 below). A few studies weakly suggest that regular ketamine works better than esketamine, although the difference is probably slight. Most of the highest-quality studies were done on regular ketamine, and it has the strongest support as a depression treatment, but I don’t want to exaggerate the difference. These are two very slightly different forms of ketamine and the differences between them are likely minor.
If you’re getting ketamine through your insurance, you’ll probably get esketamine, because insurance companies like officially endorsed things. Your doctor might also prefer giving you esketamine if they haven’t researched this topic very clearly, because pharma companies work hard to inform doctors about esketamine and work equally hard to make sure doctors don’t know that regular ketamine is an option. If this is the kind that’s most convenient for you to get, that’s fine, and you should try it and it will probably work.
If nobody is paying for your ketamine, then it becomes relevant that esketamine usually costs orders of magnitude more than regular ketamine, is harder to get, is more annoying to use, and comes in fewer convenient forms and doses. You will probably find that regular ketamine is more convenient for you, and that’s also fine, and you should try it and it will probably work.
7: What’s the right dose of ketamine?
The standard dose of IV ketamine is 0.5 mg/kg (eg 35 mg for a 70 kg person). This is the dose used in most studies and recommended by UpToDate. If that doesn’t work, some people will try going up to 1 mg/kg.
The standard dose of intranasal ketamine is 50 – 80 mg. This is more or less the dose recommended by UpToDate, the dose used in most studies, the FDA-recommended dose of Spravato, and the dose that most successful ketamine providers have told me they use.
I’m less sure that there’s a standard dose of oral ketamine. The above sources say anything from 1 mg/kg body weight, to 50 mg, to as high as 150 mg or 300 mg.
In theory, ketamine bioavailability looks like this (below table is esketamine, but racemic ketamine is similar):
IV is the best-studied route, and we know that 0.5 mg/kg is a good dose – so again, that’s 35 mg for our 70 kg patient. That would suggest that the same patient should get 70 mg nasal, 140 mg sublingual, and 175 mg orally. The 70 mg nasal seems to match the high end of prevailing practice, but the calculations for oral suggest that most prevailing practice is too low. Since different sources give different numbers for oral anyway, I would just err on the side of the higher sources.
Also, all of this is kind of arbitrary. Sometimes people will randomly give patients 800 mg doses of ketamine, and they do fine. I wouldn’t recommend this, but I can’t really say why not, except that it’s not prevailing practice, and smaller doses seem to work equally well. Remember that recreational users are taking 3,000 mg a day or higher – this doesn’t exactly go well for them, but they also don’t die immediately. My point is that ketamine is a compound with a very wide therapeutic index and you probably don’t need to panic about getting it exactly right.
–7.1: What are the exact instructions for dosing ketamine correctly?
Here are the instructions I ended up with after asking various experts who report success prescribing ketamine:
Get a compounding pharmacy to prepare a ketamine 100 mg/ml saline nasal spray solution, in an intranasal spray bottle that sprays 0.1 ml at a time (so, 10 mg/spray).
Your first few tries will be tests to make sure you respond okay to the ketamine. Have a friend sit with you for these sessions. Expect each test to take about three hours, ie that’s the amount of time you would feel bad for if you were going to have a bad reaction.
Start by spraying one spray of ketamine (= 10 mg) into one nostril. This is your first test. Wait three hours and see if anything bad happens. The most likely bad things are you feel nauseous, “weird”, or confused, or you have mild unpleasant hallucinations. Realistically the hallucinations will not happen at this dose, but check for them anyway, to make sure you’re not some kind of rare super-responder. If they do happen, try to wait it out with your friend. If something worse happens, or you’re really concerned, call your doctor - or, in an emergency, 9-1-1.
The next day, try a slightly stronger test. Spray one spray into one nostril, then wait ten minutes, then another spray into the other nostril, then wait ten minutes, then another spray into the first nostril again, for a total of three sprays (= 30 mg) over 20 minutes. Then wait three hours, as before, and see how you do.
The next day, try a full dose. This is five sprays (= 50 mg), by the same alternating-and-waiting process as before. Hopefully, 24 hours after this one you should be feeling some positive effect (ie your depression is better). If you’re not, talk to your doctor about potentially increasing your dose. If you are , talk to your doctor about how long you’re going to keep doing this for. Usually I tell my patients to take this dose twice a week for a month, then reassess – with the plan usually being to stop at that point and see whether the depression comes back vs. is gone for good.
Realistically this whole procedure is overcautious. Again, a bunch of people at raves will randomly take 1000 mg + their first time, have some crazy hallucinations, and then feel fine. I think it’s a good idea to err on the side of caution, but if for some reason this is a desperate situation or this gradually escalating process of testing doesn’t work for you, there’s no compelling medical reason why you can’t take a full dose your first time. If you have to do this, I would doubly recommend having a very trusted friend watching you.
8: How long does ketamine work for? Do I have to keep taking it forever?
Good question, currently without a good answer.
Different studies give somewhat different results for how long ketamine lasts, as do reports from expert prescribers. Median time until relapse (ie the point at which half of the people who got better after taking ketamine will be depressed again) is variously given as two weeks, four weeks, or a few months. This meta-analysis looks at four studies of ketamine effect duration; the most pessimistic finds a median time until relapse of one week, the most optimistic of one month. Here’s a pretty typical finding (source; this is based on 17 patients and yet it’s still the best I could find):
Seems pretty bad. Are there ways to make sure you stay un-depressed after successfully using ketamine?
This has been surprisingly poorly studied. A few very weak studies have shown weak positive effects from following up ketamine with cognitive behavioral therapy or transcranial magnetic stimulation. This studies are very preliminary and I don’t think it’s worth taking them too seriously at this stage. I’m also not sure whether the idea is that these have some sort of special interaction with ketamine, or whether these are just generally good treatments for depression, and doing any good treatment for depression will keep you non-depressed longer than not doing it.
In other extreme depression treatments, like ECT, a common strategy is to do the treatment, then put the patient on a traditional antidepressant afterwards to try to sustain the effect. This has not really been studied for ketamine, except one study using lithium as the traditional antidepressant (lithium monotherapy isn’t really that traditional for unipolar depression), which didn’t work. As far as I know, nobody has done any work on whether ketamine + SSRI is able to maintain remission longer than ketamine alone, which is a weird and gaping omission.
One obvious route is to just keep using ketamine regularly. This probably works. One study found that about half of people who keep getting repeated ketamine infusions stay non-depressed after a few months, which is better than you’d expect from a single course. This study supposedly is more pessimistic, but I’m unable to access full-text. Anecdotes from clinics and prescribers suggest that people often need to maintain remission by getting regular ketamine “top-ups”, usually around the order of however long it takes the ketamine to stop working. So if ketamine works for two weeks and then stops, you should probably get ketamine infusions sometime more often than once every two weeks. This is a very bad match for the traditional ketamine delivery method where you pay a clinic thousands of dollars per infusion. It’s a much better match for oral or inhaled ketamine, which is one reason I think these methods are preferable.
How long do you have to take regular ketamine? And how long can you safely take regular ketamine? There is no good evidence around this question. By analogy to other, better-studied forms of depression treatment, it would make sense to continue ketamine for six months (the average length of a depressive episode) and then go off it and see if your depression has improved on its own. If that doesn’t work, then for other antidepressants we might have you go back on them and try again every year or two, until it becomes obvious that this isn’t worth it, after which you continue them indefinitely. There is very little formal evidence about the long-term safety of ketamine. Informally, some patients have been taking it a few times a week for a few years now and seem to be doing okay, and recreational users seem to be able to handle long-term use of much higher doses. This doesn’t meet usual standards of medical evidence for establishing safety, but if the alternative is being severely depressed indefinitely, then taking your chances with regular ketamine seems like a better bet.
I can’t stress enough how poor the research is here and how little anyone seems to care about this. Ask your doctor and rely on their common sense and intuition. My personal common sense and intuition tells me that if ketamine works for recovery, it will probably work for maintenance too, and if it’s the only thing that will treat depression, it’s probably worth it.
9: What is ketamine-assisted psychotherapy?
The standard use of ketamine is purely biochemical – ketamine does something to NMDA receptors (or AMPA receptors, or whatever) and that makes you temporarily less depressed while it’s doing that.
Ketamine-assisted psychotherapy is a little different, and works more like other drug-assisted therapies (eg with LSD or MDMA). The idea is that ketamine gets you into an unusually fluid mental state where you’re able to reach insights and produce changes that would otherwise be unavailable (for a description of why this might happen, read Relaxed Beliefs Under Psychedelics And The Anarchic Brain or this review of it). Ketamine isn’t a traditional psychedelic, but it seems to produce some of the same effects.
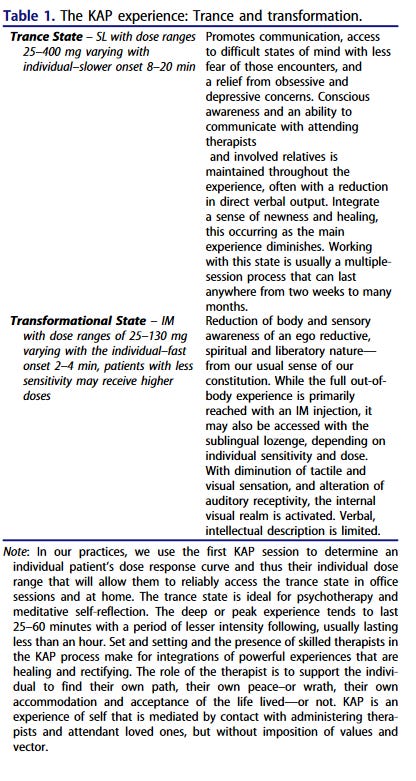
In a typical KAP session, the patient would take a high dose of ketamine – usually significantly higher than in normal ketamine treatment. Then they would lie down in a comfortable position and “form an intention” (eg “I want to understand why I feel so stuck in my job”). While on the ketamine, they would watch the flow of thoughts that came to them, holding the intention very lightly (ie not worrying or beating themselves up too much if their train of thought goes somewhere else). A therapist would sit with them, guide them, and gently ask them questions. This usually wouldn’t be some kind of very formal therapy like CBT – the goal would just be to sit with the patient as they explore their own thoughts for a few hours. This might be preceded by a few “getting to know you sessions” and followed by a few “integrating the material” sessions.
There are no good studies showing this works. Here is an open-label, no-placebo study showing it works, but everything works in open-label non-placebo studies. That having been said, many patients say it works, and there’s strong preliminary evidence for other psychedelic therapies like MDMA.
This does have some disadvantages of this over regular ketamine therapy. In order to get into a “trance” state, you have to take more ketamine than you would usually use for a purely-biological treatment. The purely biological treatment can usually be completed without you feeling anything too weird or hallucinatory or foreign to your usual mental state; the ketamine-assisted psychotherapy usually can’t. Dissociating, feeling in a trance, or having “out of body experiences” are considered standard parts of this modality.
–9.1: Where can I get ketamine-assisted psychotherapy?
Various clinics offer it all over the country. Here in the Bay Area, Polaris Health is a very well-regarded provider. They charge $950 for a single three-hour therapy session, plus extra costs for an intake session, a preparation session, etc. Overall, expect this to get well into the four digits, and don’t expect insurance to pay for it. I don’t think this is good value for money for anybody on a limited budget, if the alternative is having a doctor prescribe you inexpensive intranasal ketamine/ketamine lozenges. If your only other option is IV ketamine clinics that charge as much or more, you might as well take the free therapy (though be careful when making this calculation, IV clinic prices are often per course of ~6 sessions whereas psychotherapy prices are per session).
Sage Institute is a great organization which gives “sliding scale” treatments to less-well-off people who can’t afford the full cost, but unsurprisingly they have a long wait list.
–9.2: Can I do informal ketamine-assisted therapy on my own?
Obviously this is a sketchy idea, but how sketchy, exactly?
Several ketamine-assisted psychotherapy clinics have patients do their first session, or first few sessions, with a therapist. Then once the patient is familiar with it, they let them do further sessions at home with a friend or relative they trust.
Some people without access to a KAP clinic, but with access to ketamine, try a version of this where they skip the part where they interact with the formal medical system. Among the many disadvantages: you would have to figure out the right dose yourself (it’s different from person to person), you wouldn’t have a professional screening you to make sure you’re a good candidate for ketamine (this is mostly simple things like checking if you’re pregnant, but there are many simple things), your friend would have to call a hospital if something went wrong, and you would need to really trust your friend to be supportive and good at helping you through the experience.
(source)
Also, a common opinion among KAP providers is that ketamine is less good for this than LSD or MDMA, and is only their drug of choice because it’s legal. If you’re going to do this illegally, you might want to consider using an actually illegal substance, which could be more effective.
10. How does ketamine work?
Currently this is very poorly understood.
Ketamine is a very strong antagonist of NMDA receptors, one of the key excitatory receptors in the brain. That is, most of the time when neurons want to tell other neurons to be more active, they release a chemical called glutamate, which is detected by NMDA receptors, which activate the neuron. Since ketamine antagonizes these receptors, it prevents neurons from being activated – although, just to make all this more complicated, many neurons suppress other neurons, and when these neurons are less active, it makes other neurons more activate. For many years, scientists assumed that somehow all of this had something to do with ketamine treating depression, although nobody was really sure how, and other NMDA receptor antagonists didn’t seem to treat depression at all. My impression is that this theory is now on thin ice, and that the people who keep repeating it aren’t really up to date on the research.
Over the past few years, increasing evidence suggests that ketamine (or possibly its metabolite hydroxynorketamine) activates a different glutamate receptor called AMPA. Activation of AMPA leads to various changes in the cell (like activation of mTOR and release of BDNF) which promote increased synapse strength. Since depression is plausibly a condition of decreased synapse strength, or imbalanced synapse strength in different parts of the brain, this increase in synapse strength helps treat depression. You can read a very technical presentation of some of these ideas here.
Other theories include that ketamine is secretly an opioid and maybe opioids treat depression for some reason (based on this study, but contradicted by this study, and I think no longer really plausible), that ketamine is a really impressive placebo (I think contradicted by eg mouse studies, studies with active placebo comparator, etc, but some smart people still believe this) and that it’s a really complicated combination of all sorts of things we’ve barely begun to understand (almost certainly true).
11. Will you prescribe me ketamine?
I sometimes prescribe patients ketamine, but I prefer not do to do this until they’ve tried a few traditional antidepressants first to see if that’s enough.
Why? First and foremost, because although I’m optimistic about ketamine, it’s new and poorly understood, and anything which is new and poorly understood has higher risk of having some side effect we don’t know about. Second, because the effects of ketamine wear off quickly unless you continue taking it indefinitely, and continuing ketamine indefinitely is very poorly understood and makes me nervous. Third, because even if you use regular ketamine from a compounding pharmacy (the cheapest method) it’s going to be more expensive than other medications and not covered by insurance, and if you need to pay for this expensive thing indefinitely it will be very expensive, and I would rather you start by taking another antidepressant which you can use indefinitely for much cheaper. Fourth, because the government controls ketamine pretty carefully, this is bad for me insofar as I have to convince the government I’m not dispensing it irresponsibly, and it’s bad for you insofar as you have to navigate the bureaucracy around picking up a controlled substance, which is much harder than picking up a regular medication. And fifth, because although the risk of getting addicted to ketamine is low, it can happen, especially if you take it indefinitely, and I’d rather start with antidepressants that don’t have that risk.
If you’ve failed many other medications and have severe depression, I’m happy to work with you in investigating other strategies, and ketamine might be one of them. I would prefer patients not join my practice just to get ketamine, and you should be prepared for me not to give it to you if I don’t think it’s the best choice.