Zounds! It's Zulresso and Zuranolone!
1: What is Zulresso?
Wikipedia describes Zulresso as “A bat-winged, armless toad with tentacles instead of a face… ” - no! sorry! That’s Zvilpogghua, one of the Great Old Ones from the Lovecraft mythos.
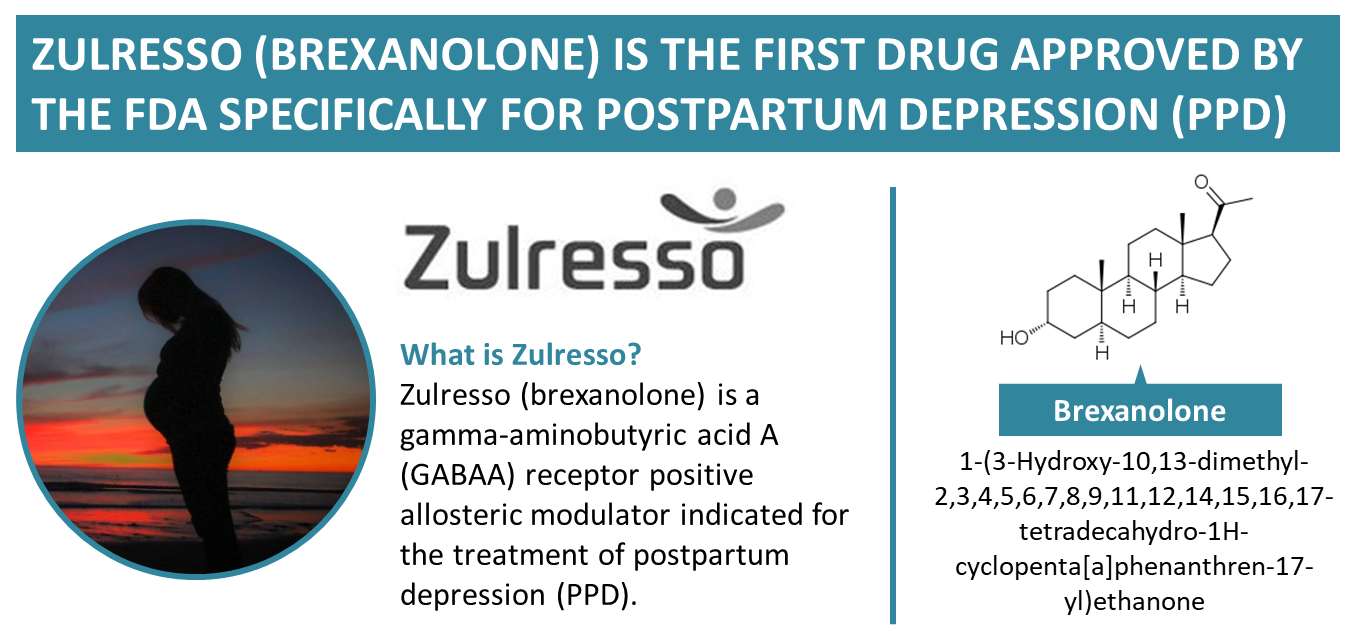
Zulresso is the brand name of allopregnanolone (aka brexanolone), a new medication for post-partum depression. It’s interesting as a potential missing link between hormones and normal mood regulation.
2: What do you mean by “missing link between hormones and normal mood regulation?”
Allopregnanolone is a naturally-occuring metabolite of the female hormone progesterone. In 1981, scientists found it was present in unusually high concentrations in the brain (including male brains), suggesting that maybe the brain was making it separately and using it for something.
They did some tests and found that it was a positive allosteric modulator of GABA.
| [](https://substackcdn.com/image/fetch/f_auto,q_auto:good,fl_progressive:steep/https%3A%2F%2Fbucketeer-e05bbc84-baa3-437e-9518-adb32be77984.s3.amazonaws.com%2Fpublic%2Fimages%2F4195b6ed-7ab4-45bb-83c6-052c067e434c_1355x639.png)(source) |
GABA is the main inhibitory neurotransmitter; it’s usually associated with relaxation and sedation. A positive allosteric modulator is a chemical that makes receptors respond more strongly to their targets. So “a positive allosteric modulator of GABA” means a chemical that makes the brain respond stronger to relaxation/sedation signals. Sounds pretty useful! You may do some positive allosteric modulation of GABA yourself sometimes; this is one of the major actions of alcohol. Also of the benzodiazepines, a popular class of psychiatric medication including Ativan (lorazepam), Valium (diazepam), and Klonopin (clonazepam). The “-pam” at the end stands for p ositive a llosteric m odulator!
(or maybe that’s just an urban legend, I’ve never found proof either way)
The discovery of endorphins (ie endogenous opiates) helped shed light on the brain’s reward system. So the discovery of a sort of endogenous benzodiazepine was pretty exciting. Maybe it’s some kind of master control switch for anxiety or something?
Psychiatrists only know two ways to respond to an exciting new thing: publishing breathless studies claiming that it’s the true mechanism of action for SSRIs, and publishing breathless studies claiming that it’s the true biological basis of depression. This time, they did both: see eg Fluoxetine elevates allopregnanolone levels in female rat brain and The role of allopregnanolone in depressive-like behaviors. The basic theory was that stress / social isolation / etc → decreased allopregnanolone → something something BDNF and synaptogenesis → depression. And SSRIs → increased allopregnanolone → something something BDNF and synpatogenesis → recovery!
Change the word “allopregnanolone”, and that’s every theory in psychiatry. But this particular theory had two extra pieces of evidence: premenstrual dysphoric disorder and postpartum depression.
Remember, allopregananolone is a natural metabolite of the female hormone progesterone. Progesterone levels go up during pregnancy and the ~18th day of the menstrual cycle, then crash back down after delivery and the ~24th day of the menstrual cycle. Meanwhile, some women get depressed after delivering a baby, or on the ~24th day of their menstrual cycle. Suspicious! Maybe it’s because their progesterone was getting converted into allopregnanolone, an antidepressant hormone that affects mood!
(why doesn’t every woman get PPD and PMDD? This study suggests that women with PMDD have altered sensitivity to allopregnanolone; plausibly people with PPD have some other form of altered sensitivity. In case you have the same question I do: the correlation between PMDD and PPD is not 100% but still pretty significant)
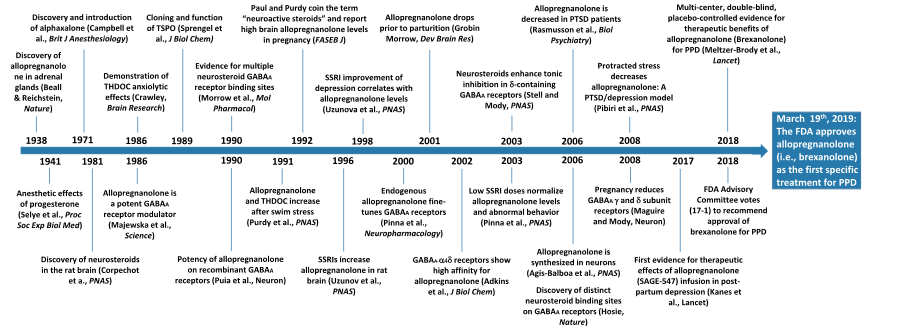 History of allopregnanolone research (source)
History of allopregnanolone research (source)
The next step was to see if making patients take allopregnanolone can treat these conditions. This is kind of hard, because allopregnanolone is a tough chemical to get into people’s bodies; the traditional method involves sticking an IV into someone and infusing it slowly over several days, and it has to be done in a hospital. Still, Kanes et al tried this in 2017. The study was open-label (ie no placebo) and very small (only four women) but appeared to work extraordinarily well. Four post-partum women who qualified as “severely depressed” when they started the infusion progressed to “completely recovered” within twelve hours. Nothing else except maybe ketamine had produced results like this before.
3: What studies were done on Zulresso?
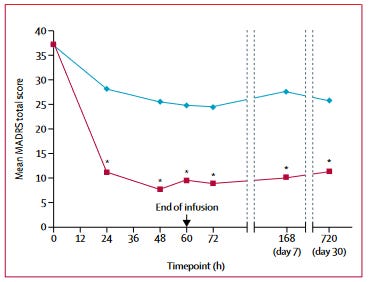
This followup study by Kanes was the first real RCT, although it only had 21 patients. In accordance with the venerable First Study Ever tradition, it found really large positive effects on post-partum depression.
That encouraged Sage Therapeutics to fund a bigger Phase 3 trial, Meltzer-Brody (2018). In accordance with venerable Bigger Phase 3 Trial tradition, its results weren’t quite as good as the First Study Ever. But they were still pretty good:
Notice that lower doses worked better than higher doses. This is sometimes a red flag on a study. But this time it seems legit; see “Biphasic Actions At The GABA-A Receptor” here for an explanation.
Both studies also evaluated side effects. These were generally mild, but two people (about 2% of the study population) lost consciousness. Nothing seemed wrong with them, and researchers mostly attributed this to allopregnanolone being a sedating drug. If you sedate people too hard, they pass out.
Faced with these results, the FDA approved allopregnanolone for post-partum depression, but subjected it to a REMS (Risk Evaluation And Mitigation Strategy) - basically, doctors who want to prescribe it will need to take special courses and do extra paperwork.
This kind of surprised me - there are plenty of sedating drugs that make you pass out in overdose. Also, since patients will be getting it IV, there will probably be a nurse around to check if they passed out and take appropriate actions if so. But the FDA really likes putting restrictions on things, and I guess this was a free chance for them to do that.
4: Is Zulresso freely available at a doctor’s office near me?
It’s possible to get Zulresso, but really hard.
Because Zulresso is an IV infusion lasting four days, you need to spend four days somewhere that people can put an IV into you and monitor it. Realistically that means a hospital or some other big medical institution. So this is only available for inpatients.
Because of the REMS (extra certification and paperwork), most hospitals aren’t interested. You can find a list of ones that are here - it looks like there are about 89 locations in the US with the right certification.
Last but not least, a four-day course of Zulresso costs $35,000 for the medication itself, plus much more for the four-day hospitalization it takes to receive it. As usual, insurances will cover it iff you can document you’ve tried lots of other stuff first.
5: Hold on, does it really cost $35,000?
Oho, I see you’ve played the “pharma price analysis” game before.
But this time I think the price might actually be defensible. Chemical supply companies (1, 2, 3) generally sell allopregnanolone for $10,000 to $20,000 a gram.
(I found one company with a much lower price, but I’m suspicious and am going to dismiss them as an outlier).
The usual dose of allopregnanolone is 60 ug/kg/hour x 60 hours, which for a 60 kg person comes out to a total of 0.25g total. Getting that amount from the chemistry supply store would cost about $2,500 - 5,000. I assume pharma-grade allopregnanolone is more expensive than chemistry-store-grade, so it wouldn’t surprise me if a price in the low five-figures was justified by manufacturing alone.
Isn’t it still a pretty good deal to find an endogenous neurosteroid, do one or two studies confirming it’s great, produce it for the low five figures, then sell it for the mid five figures? I think maybe not. This drug has a terrible value proposition. Post-partum depression is one of the rarer psych conditions. Most people with PPD won’t check into a hospital and pay $35,000 for a drug infusion. And the people who do will get the drug infusion, feel better, and never need it again (at least until they have another kid) - unlike SSRIs where you can keep charging for monthly prescriptions forever.
Sage Therapeutics, the pharma company that owns the patent on Zulresso (and nothing else - this is their only drug!) has done terribly. Their stock is in the doldrums, they almost went bankrupt, and they survived only with the help of a cash infusion by a bigger pharma company.
I think this confirms a general trend where at least some expensive medications are pricey because of fundamentals (including regulatory fundamentals) and not just pharma companies making obscene profits.
6: Hold on, how is allopregnanolone different from benzodiazepines?
Remember, allopregnanolone is a positive allosteric modulator of GABA, much like benzodiazepines such as Xanax. But Xanax is cheap ($10 for 30 pills). And you can get it at any local pharmacy (plus sometimes on street corners). What’s so special about allopregnanolone that you should pay $35,000 and go into the hospital to get it?
The official answer is “allopregnanolone modulates GABA differently from benzodiazepines”. For example, this paper says that:
Allopregnanolone allosteric modulation of the action of GABA at GABA-A receptors is much less selective than that of benzodiazepines, which are relatively inactive at α4- or α6-containing GABA-A receptors.
If you really like details about receptor subunits, this paper presents the full case.
The skeptic’s answer is “who knows?” Psych drugs often work for reasons totally different than we thought. People thought tianeptine was an SSRE for years, until it turned out to be a mild opioid. People thought ketamine was NMDA-ergic for years, until it turned out to be [fill this part in 10 years from now]. Last year a bunch of very smart people tried to claim that SSRI effects had nothing to do with serotonin (I think they were wrong). Just because some guy found that Zulresso acts as a GABA-PAM in some test tube doesn’t mean that’s what’s having any of the relevant antidepressant effects.
The troll’s answer is “who says it’s different?”
Do benzodiazepines treat depression? Depends who you ask. If you ask benzodiazepine users, their answer is “yes, definitely”. If you ask drug warriors, their answer is “Addictive Substances May Make You Temporarily Feel Good, But They Are Not A Responsible Treatment Option”. If you ask the research literature, it gives vague indeterminate answers, as always.
But nobody has ever said benzodiazepines instantly and miraculously cure depression, so how come allopregnanolone seems to do that? A true troll would point out that we probably give allopregnanolone at much higher doses - 2% of allopregnanolone patients were sedated so hard they lost consciousness, whereas this is exactly the sort of side effect I try to avoid when calculating benzodiazepine doses. Maybe if you gave postpartum women an infusion of 300 mg Valium, and maximized your placebo effect by calling it the hot new thing, they’d do pretty well too (several days later, after recovering consciousness).
I think the troll answer would be hilarious but I don’t really want to defend it as correct; if I had to bet I’d say the official explanation is the right one.
7: Hold on, why can’t we just give people progesterone and let them metabolize it into allopregnanolone?
This turned out to be an interesting enough rabbit hole that I’m going to spin it off into another post later this week.
8: Hold on, people have lots of allopregnanolone when they’re pregnant, right? And then post-partum depression happens when they give birth, and their allopregnanolone level drops. So if you give someone an infusion of allopregnanolone, and then take them off it, that’s a hormonal simulation of giving birth, ie the same thing that caused the problem in the first place? How is that good?
Oh, you think you’re clever, do you? What you failed to consider is . . .
I didn’t end that sentence because I can’t find anything in the literature addressing this question. But the difference might be that the infusion schedule ramps up gradually, peaks, and then ramps down gradually, which is more of a soft taper than the sudden crash of birth. If anyone knows more about this, please let me know. [EDIT: see this comment]
9: Is allopregnanolone addictive?
No, because good luck getting addicted to a $35,000-per-dose chemical.
We should probably expect allopregnanolone to be addictive, by analogy to other GABA-PAMs like benzodiazepines and alcohol. But nobody has ever received more than a single dose. You don’t get addicted to benzos after a single pill, or alcohol after a single beer, so in practice AFAIK nobody has ever gotten addicted to this.
Or who knows, maybe it’s not addictive. Remember, allopregnanolone is naturally elevated during pregnancy; pregnancy isn’t addictive. And some scientists claim the brain endogenously uses allopregnanolone as a master regulator of depression and anxiety. In theory , if you could give yourself the same amount a non-anxious person’s brain gives them all the time, shouldn’t you be no worse off than that non-anxious person? I don’t know, and remember that your brain also has a lot of endogenous opioids; doesn’t make the exogenous kind any safer.
The Drug Enforcement Administration has made Zulresso a Schedule IV controlled substance, which means they’re putting a few very weak restrictions on it but not worrying too much.
10: Does allopregnanolone work for depression that isn’t post-partum?
If all psychiatric disorders are secretly allopregnanolone imbalances, then you might expect it to work on all depressions, not just post-partum.
I’m sure pharmaceutical executives with dollar signs instead of pupils in their eyes have had this same thought, but I can’t find studies about it.
Some of the same people behind the postpartum studies did a very small, very weak study on ganaloxone (a close allopregnanolone relative) for persistent depression; it seemed to work, but also caused a lot of sedation (more than in the postpartum trials? Hard to tell). Nobody’s looked into this further since then, maybe because that was around when the pharma companies realized that the 4-day hospital stay and $35,000 price tag made allopregnanolone a financial loser.
The evidence from zuranolone (see below) suggests that allopregnanolone might not work very well against regular depression.
11: What is zuranolone?
Wikipedia describes zuranolone as “a swirling, black vortex revered by the Mutsune Native Americans as a dire death god . . . also worshiped by mysterious servitors known as the Hidden Ones .”
No! Sorry again! That’s Zushakon, another Great Old One. Zuranolone is Sage Therapeutics’ attempt to turn allopregnanolone into an accessible medication that might actually make them real money.
 Zuranolone is mostly just allopregnanolone with some extra stuff attached that changes the absorption.
Zuranolone is mostly just allopregnanolone with some extra stuff attached that changes the absorption.
Zuranolone can be taken orally, so you don’t have to go to a hospital for four days to receive it IV. It’s potentially less likely to cause loss of consciousness and other undesirable side effects. And it’s under investigation as a potential treatment for postpartum depression, bipolar depression, regular depression, insomnia, and various movement disorders.
(that might seem excessive, but benzodiazepines treat a lot of stuff, and if these neurosteroids are kind of like super-benzodiazepines, then this level of optimism might be warranted.)
12: Does zuranolone work?
Sage Therapeutics answered this question the same way pharma companies answer every question: with a bunch of studies whose names form overly-cute acronyms. We’ll talk here about ROBIN, WATERFALL, MOUNTAIN, and CORAL - though I assure you there are others.
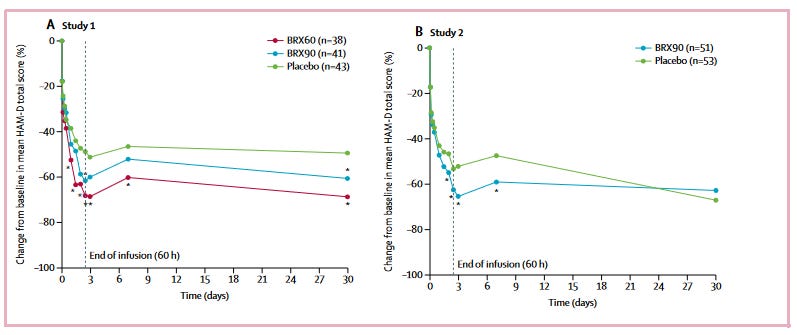
ROBIN tested efficacy in postpartum depression. Results were positive and relatively impressive, about the same as the weaker allopregnanolone studies.
WATERFALL, MOUNTAIN, and CORAL tested results in regular depression. WATERFALL was positive but weak. MOUNTAIN was negative. That scared the pharma company and they hacked CORAL to be more likely to give positive results. It did give positive results, but the FDA reads the same biotech magazines I do and knows perfectly well what they did, so I don’t know what Sage expects to gain from this. Overall these trials were disappointing.
I think the most likely story is that allopregnanolone = zuranolone, both are moderately effective in postpartum depression, and both have much less efficacy in regular depression, probably not literally zero but also not enough to be worthwhile antidepressants (especially considering cost).
Might zuranolone be an excellent anti-anxiety medication? You’d think so - it should be at least as good as benzodiazepines, which are excellent anti-anxiety medications. And researchers seem excited about allopregnanolone as a master regulator of brain anxiety. But the studies aren’t promising. ROBIN and WATERFALL incidentally assessed anxiety; ROBIN found good results in its postpartum population, but WATERFALL found poor-to-mediocre results in its regular population.
Studies are hard, and sometimes even really effective drugs can have trouble showing strong results. But these aren’t encouraging.
13: So where do we go from here?
Getting FDA approval for zuranolone for postpartum depression seems reasonable; it’ll probably be cheaper and easier than making people go to the hospital to get allopregnanolone. I’m uncertain about the financials of this for Sage, but since they did the study they hopefully think it’s worth it.
Otherwise, I’m not sure. It would have been great if zuranolone had shown robust efficacy against regular depression and anxiety, but this is exactly the kind of great thing that never happens in psychopharmacology (motto: “Disappointing Doctors And Patients Since 1982”). It might be worth throwing it against anxiety disorders and PTSD to see if anything sticks, but I wouldn’t bet on it.
The research into allopregnanolone as master regulator of brain anxiety states is fascinating, but as far as I know it hasn’t reckoned with the failure of zuranolone to really treat much anxiety. The cynical part of me predicts that once pharma’s done making money off neurosteroids then all of this will die down, and something else that pharma can make more money from will become the master regulator of everything.
I expect that the main thing we get out of all this is somewhat better post-partum depression treatment, which might or might not ever become accessible for ordinary people.
14: Predictions
In the next five years…
-
Zuranolone gets FDA approval for major depression: 15%
-
Zuranolone gets FDA approval for postpartum depression: 45%
-
Zuranolone gets FDA approval for some other condition: 33%
-
Another neurosteroid gets FDA approval for a psychiatric indication: 35%
-
Researchers become more convinced that allopregnanolone is an important regulator of brain anxiety states (at least as important as serotonin): 40%
-
The scientific consensus is still that allopregnanolone works by modulating GABA receptors in a way importantly different from benzodiazepines: 90%